With the popularity of wearable devices such as smart watches and health bracelets, more and more products use optical heart rate sensing technology (PPG, photoplethysmography) to monitor users' heart rate, blood oxygen and other physiological data. However, the measurement results of such optical sensors are easily affected by various factors such as ambient light, skin color, and wearing method, resulting in uneven data accuracy.
Therefore, the industry needs a set of "gold standards" as a benchmark for testing and calibration, that is, a "recognized, traceable and highly accurate reference standard" to evaluate the PPG sensing performance of wearable devices. This standard ensures the consistency and reliability of test results, so that products can be strictly and objectively verified during the design, development and mass production process.
Simply put, the gold standard is a "ruler" used to measure the accuracy of PPG data of wearable devices, ensuring that each device can achieve the expected quality and performance, thereby enhancing consumer trust in the product.
Since the gray card test commonly used in the past can only preliminarily check the optical path or signal-to-noise ratio (SNR), it is impossible to verify the measurement accuracy of single component abnormalities or physiological parameters, and it is difficult to ensure the consistency of each batch of products. Establishing a "gold standard" can make the test results measurable and traceable, ensuring that the product is accurate in all scenarios.
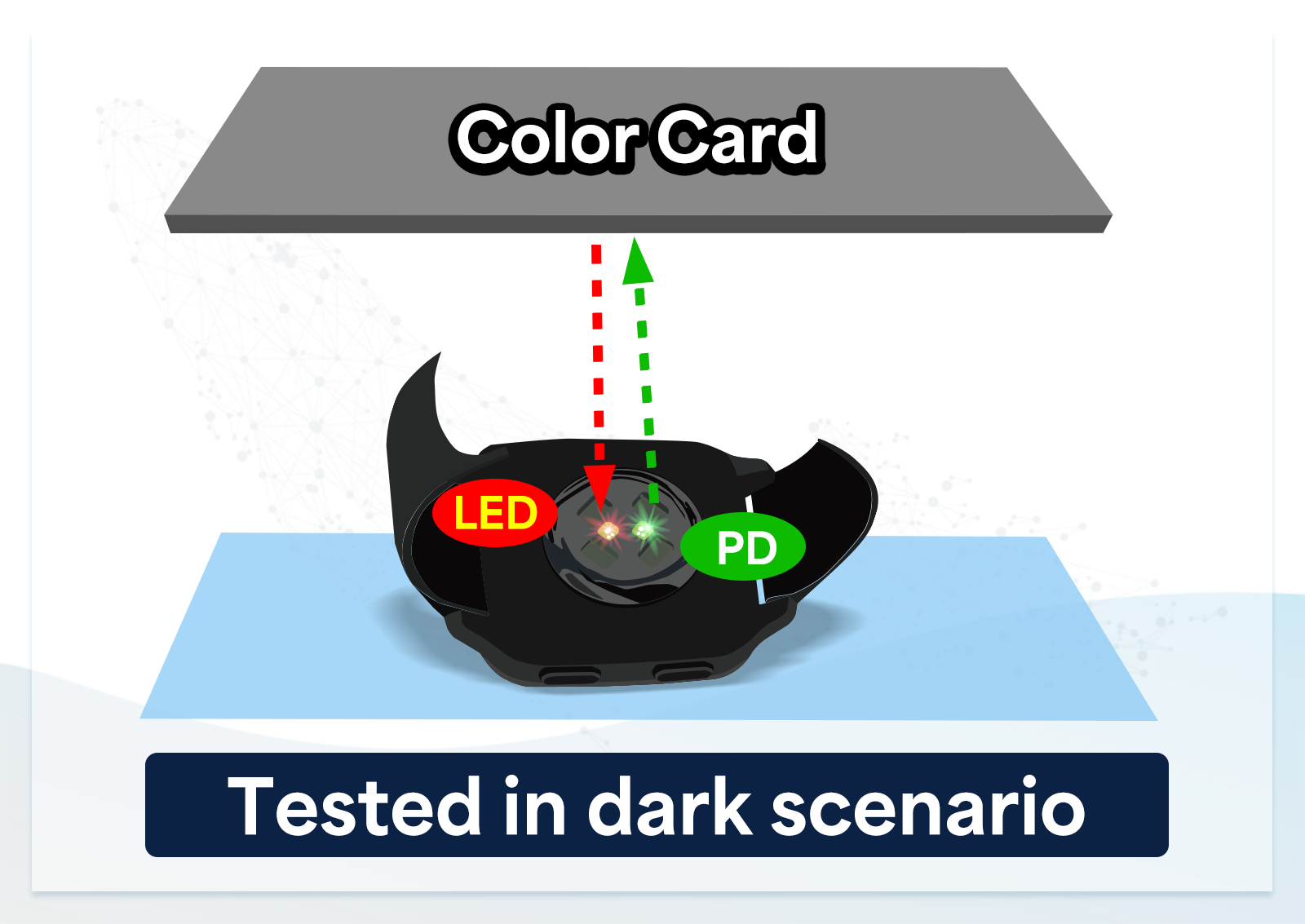
Figure: The gray card test can only evaluate the overall optical combination performance and can't determine the abnormality of a single component.
- Design verification (Before & After): Whenever the product design changes (such as replacing the sensor element, optimizing the algorithm), the gold standard can be used to repeatedly test the new and old designs to ensure that the optimized product does not deviate from the precise target.
- Mass production calibration: During the mass production stage, the gold standard can be used to calibrate each batch of products to ensure consistent accuracy, and the testing equipment can also be calibrated regularly to maintain long-term stability.
There are two main sources of gold standards:
- Clinically validated products: devices that have been proven to have accurate measurement data through clinical trials. Through the AECG100 optical performance simulator of WhaleTeq, the reference curves (called R curves) measured by these devices in a fixed test environment are recorded as a basis for comparison of mass-produced products in the future.
- Self-tested products: manufacturers define gold standards based on their own designs and needs, and can also use simulators to obtain reference R curves as internal quality control and calibration standards.
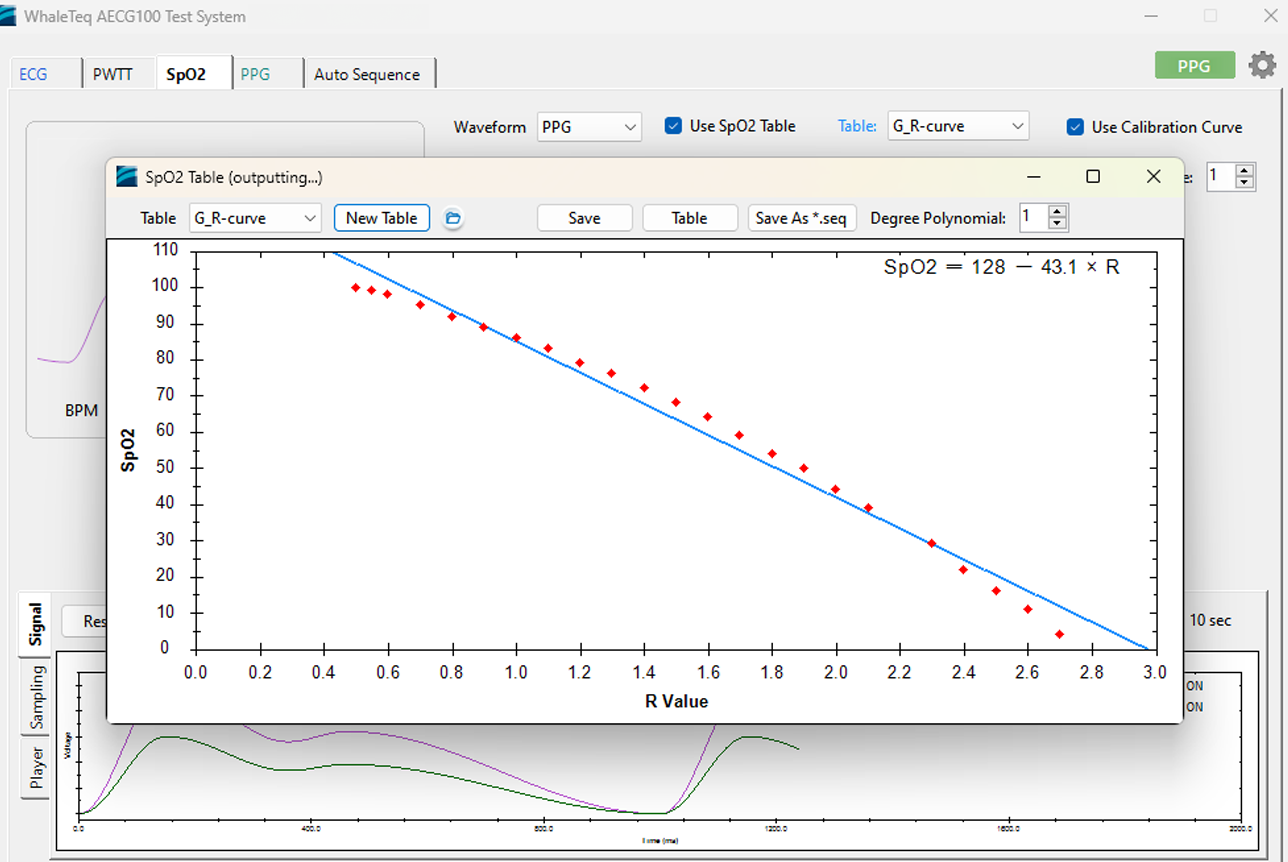
Figure: Obtaining a reference R curve through AECG100 as a basis for comparison of mass-produced products.
The AECG100 cannot simulate different ambient light conditions at this version. Alternatively, the AECG100 has data playback function, which offers users to record their self-collected waveform with different ambient light conditions and then play these recorded waveforms back from the AECG100 to simulate such condition.
After setting properly, the AECG100 is a fixed intensity output, and the output intensity does not support the corresponding DUT LED intensity change.
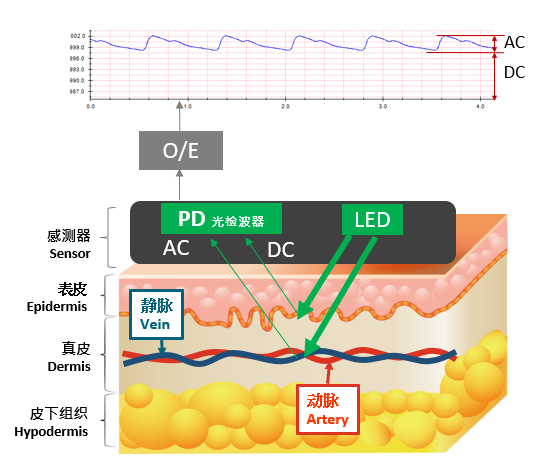
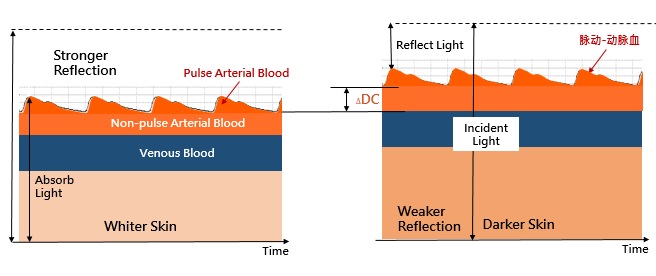
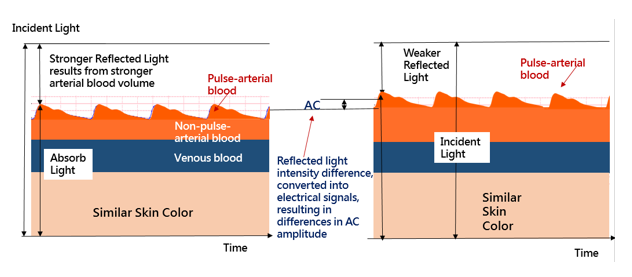
People with darker skin will absorb more incident light, so the reflected light is weaker. Due to the fact that skin, tissues and veins do not change in volume with heart beat at a steady state, the intensity of the absorbed light and reflected light is stable, converted to direct current (DC) through a photodetector (PD). Therefore, if the simulator can emit different intensity LED light, then it can achieve the goal to simulate different user skin tones. AECG100's PPG module provides users to adjust different DC levels to emit different LED intensities.
At the same time, arterial blood volume changes when heart beats. We can refer the arterial blood volume change as an alternating current (AC) signal comparing to the larger DC signal. AECG100 also provides the capability to allow users to adjust the AC level to simulate different arterial blood volume.
The first possibility is the position between the AECG100 and DUT. Or to be more specific, the DUT's LED and the tester's PD are not talking to each other due to position problems. Here are some examples:
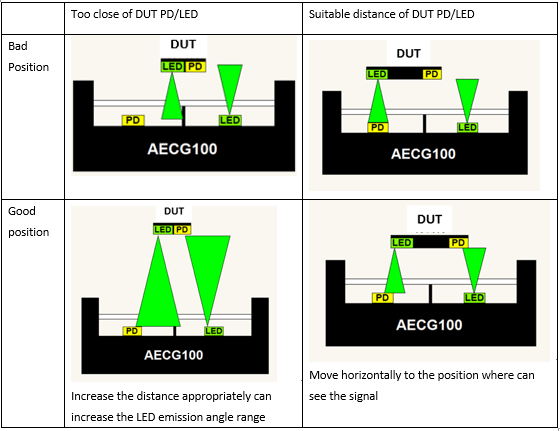
Because of the LED emission range and mechanism issues, it may be necessary to adjust the DUT location to the position where the signals can be seen.
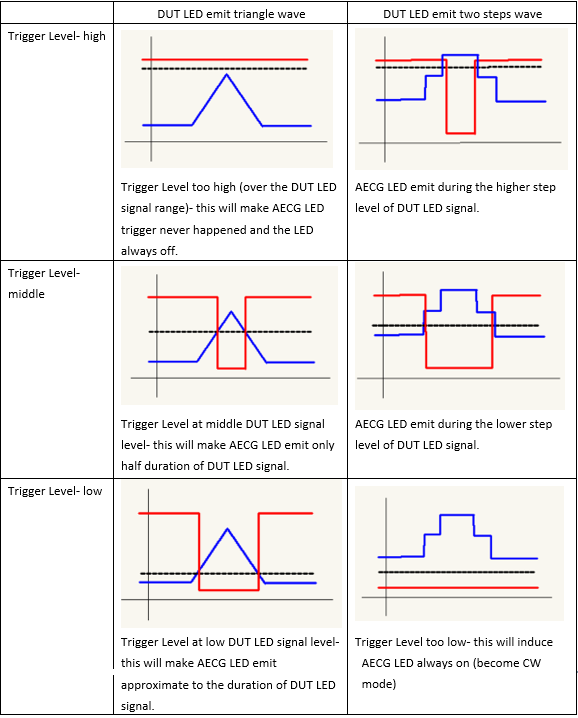
AECG100 trigger level is the threshold level to trigger AECG100 LED on (emit the light), through a LED switch to control AECG100 LED on/off. If trigger level over DUT LED signal range, it will induce AECG100 LED not to emit the light. If it's under the range, it will induce AECG100 LED always emit the light (become CW mode). Both conditions will make the DUT have no responses to AECG100 LED behaviors. Therefore, the appropriate trigger level is important for some no respond conditions. Please refer to the table below:
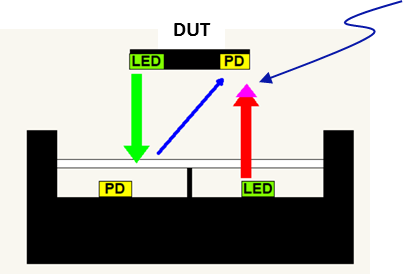
As shown above:
Blue arrow represents the DUT reflection light or outside ambient light which be reflected by AECG100 mechanism.
Red arrow represents AECG100 LED emit light (DC part)
Pink arrow represents AECG100 LED emit light (AC part)
Therefore, the light received by DUT PD can be simply as shown in the following figure (the AC/DC amplitude is not proportional, actual AC amplitude is much smaller than DC amplitude).
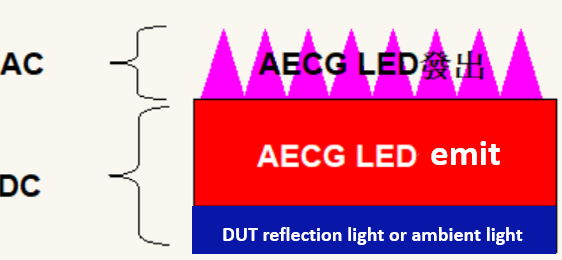
If the blue area is very small (compared to the red area) or is constant (predictable level and can be deducted from the red area), which will not cause interference.
When the application is single color light (such as green light), DC is a fixed value and the blue part is not deducted from the application. It doesn't affect the test too much.
SpO2 value is related to the ratio of R(PI)/IR(PI), PI= AC/DC, for different wavelengths of light and mechanism, the ratio of the red to the blue area is different, so it can't make the blue area small enough to ignore it (isolate the reflection light), or to be able to accurately deduct the predictable level in advance, will cause a large error in SpO2 calculation.
